Written by Arshnee Moodley and Ekta Patel
With over two million people infected with the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and almost half of the world’s population under lockdown, the effects of the coronavirus disease (COVID-19), which is caused by SARS-CoV-2, on our global community have been immediate and profound. Many countries are scrambling to source crucial medical supplies, hospitals are battling to cope with the high admissions of thousands of patients and critical healthcare systems are stretched beyond their capacities. This pandemic has called on all governments, international organizations, the private sector and the public to play a role in its containment.
While the number of COVID-19 infections in Africa does not rival those seen in Europe or America, they are gradually increasing and so is the fear of the impact this infection may have on the continent’s low- and middle-income countries (LMICs). According to the World Bank, nearly 645 million people live in the rural areas in sub-Saharan Africa. Three quarters of this population lack the facilities at home to wash their hands with soap and water, which is one of the key measures of preventing infection and spread of SARS-CoV-2. Moreover, many people in LMICs are already battling malnutrition and other endemic infectious diseases, which raises the question of how they will cope with the COVID-19 pandemic.
The delayed arrival of COVID-19 on the African continent gave governments in these countries an opportunity to start implementing preventative measures to reduce community infections when just a few cases were detected. In Kenya, for example, after the first confirmed case of COVID-19 was reported on 13 March 2020, the government responded by implementing quick preventative measures to reduce transmission. People were advised to work from home, schools and universities were closed, international travel was prohibited, county borders were closed to restrict movement, public transport restrictions were implemented, and the government began advocating for frequent handwashing and physical distancing. In countries like Uganda and South Africa, strict lockdowns have been implemented with people instructed to stay at home, leaving to purchase only essential items or seek medical care. Nearly 33 of the 54 countries in Africa have some form of regional or national lockdown.
Viral respiratory infections like those caused by SARS-CoV-2 can be complicated by secondary bacterial infections – an additional infection in individuals who already have another infection. These secondary infections are important and often fatal complication. The virus weakens the immune system making it easier for a bacterial superinfection. In the 1918 and 2009 influenza pandemics, more than 50% of deaths could be attributed to secondary bacterial pneumonia highlighting the risks associated with bacterial secondary infections.
SARS-CoV-2 is no exception. A retrospective study published in The Lancet about the outbreak in Wuhan, China, noted that of the patients who died from COVID-19, approximately 50% had a secondary bacterial infection. While all patients were prophylactically treated with antibiotics, it remains unclear if death was attributed to ineffective antibiotic treatment due to antibiotic resistance or the poor condition of the patients too weak to fight the infections. Researchers globally are currently exploring the links between COVID-19 and AMR, but it is unlikely that the exact role of antibiotic resistance will ever be known for COVID-19. This is due to the overwhelming mortality rate per day; in some countries hundreds of people die daily and coupled with the lack of post-mortem examinations, the exact cause of death will not be known.
Antibiotics play a pivotal role in a pandemic both as prophylaxis – to prevent bacterial infections – as well as pre-emptive treatment of secondary bacterial infections, which can be difficult to distinguish between viral pneumonia and bacterial pneumonia. This use of prophylactic or pre-emptive use of antibiotics in hospitalized patients will select for antibiotic resistance in the long-term negating any short-term benefits, moreover, underscoring the need for effective antimicrobial stewardship.
To determine which antibiotics would be effective as first line or empiric treatment choices in the absence of a laboratory diagnosis, requires country- or regional-specific knowledge on antibiotic resistance trends in key bacterial respiratory pathogens, which is achieved by annual collection of antibiotic resistance surveillance data. According to the World Health Organization (WHO) 2018/2019 survey on global monitoring of countries progress on addressing AMR, no country in sub-Saharan Africa noted having a functional national surveillance system for AMR in humans covering common bacterial infections in hospitalized and community patients, making it very difficult to develop effective treatment guidelines.
WHO lists antibiotic resistance as one of the ten greatest human health threats and the review on antimicrobial resistance by Jim O’Neill indicates 700,000 people die annually as a result of an antibiotic resistant infections with the most affected in LMICs. This clear geographic distinction is also reflected in the distribution of antibiotic resistance genes identified through a surveillance of urban sewage systems. Countries in Asia, Africa, and South America having higher levels than countries in Europe and North America. Antibiotic resistant bacteria can be found in people, animals, food and the environment and know no boundaries. This public health and agricultural sector challenge also affects human development as it is intimately linked to inefficient disease control, poor animal husbandry, inadequate sanitation, inappropriate food handling and socio-economic growth. These factors inadvertently affect LMICs and their attainment of the UN Sustainable Development Goals.
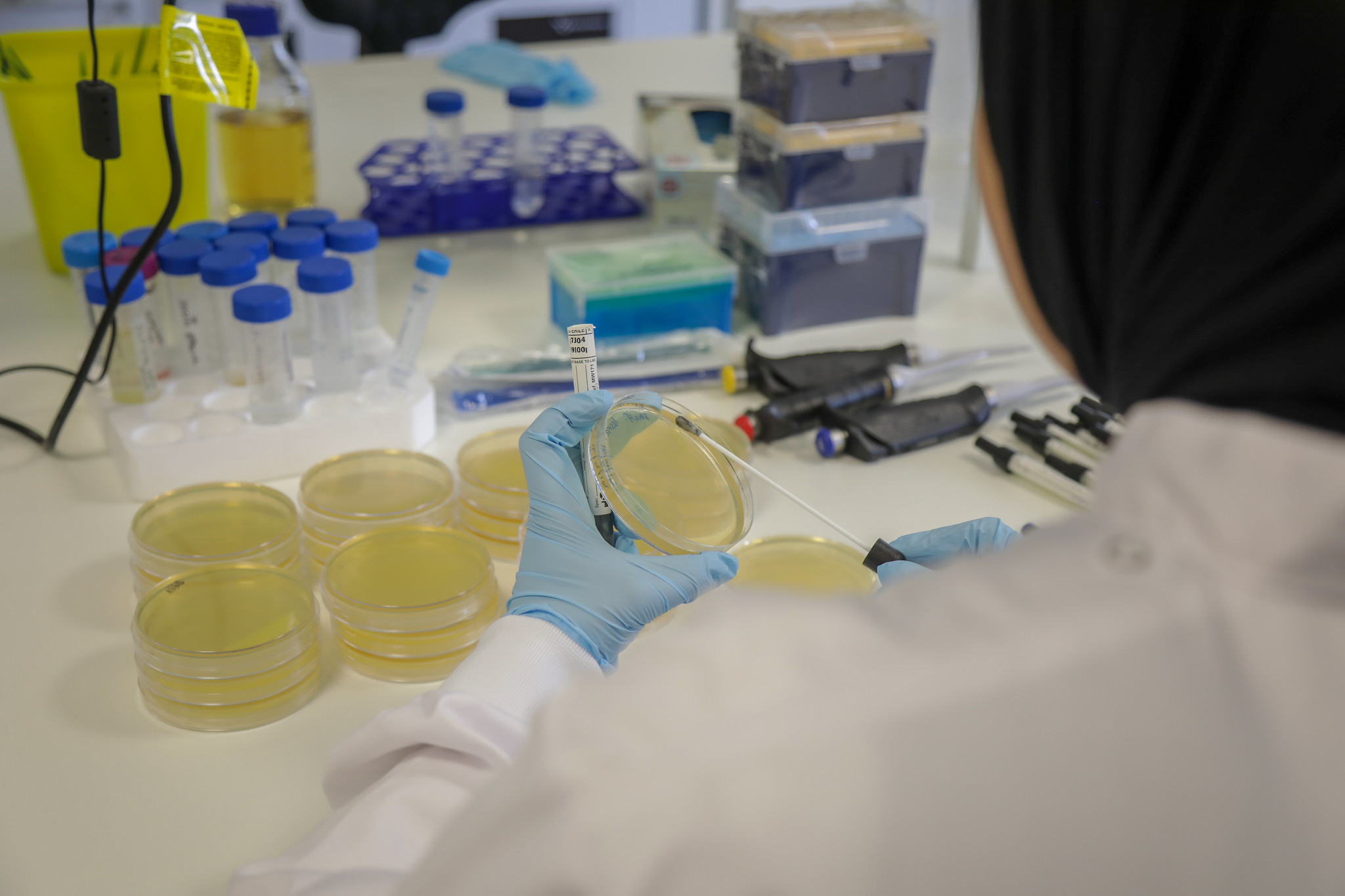
Launched in 2019, the CGIAR Antimicrobial Resistance Hub, which is led by the International Livestock Research Institute (ILRI), is focused on mitigating agricultural associated AMR risks using a One Health framework with transdisciplinary partnerships, to promote sustainable agriculture and improving human health in LMICs. The emergence and rapid spread of COVID-19 highlights the importance of diagnostic testing, which is also important for antibiotic resistance and successful treatment outcomes. The Antimicrobial Susceptibility Testing (AST) facility at the CGIAR AMR Hub, in partnership with the International Centre for Antimicrobial Resistance Solutions (ICARS) in Denmark and the European Committee on Antimicrobial Susceptibility Testing Development Lab (EUCAST EDL) in Sweden, is focused on providing robust AST testing and enhancing capacity development in LMICs. In addition, ILRI is leading the animal component of the Fleming Fund Kenya country grant and together with national partners has established a sustainable national AMR surveillance system.
For more information on CGIAR AMR Hub visit the website follow us on twitter here